|
|
|
|
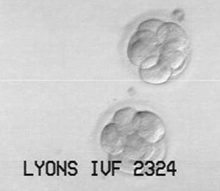
Facts About Embryos |
|
|
|
|
|
|
|
|
 |
|
|
|
| "Today a new sun rises for me; everything lives, everything is animated, everything seems to speak to me of my passion, everything invites me to cherish it..." |
|
| -Anne de Lenclos |
|
|
|
|
|
|
|
|
|
|
|
|
|
 |
|
| Embryo Facts |
|
Want to learn about embryos? Learn some of the answers to some of the most Frequently Asked Questions here.
|
| FAQ |
|
|
|
|
How are embryos created during an In Vitro Fertilization cycle?
In Vitro Fertilization (IVF) involves stimulating a woman’s ovaries to produce more than one egg through the use of fertility medications. As the eggs are developing, the woman is monitored through blood tests and ultrasound. When her two largest follicles reach the optimal size, she is given an injection of hormones to trigger ovulation. 36 hours later, the eggs are retrieved through a minor surgical procedure performed under light sedation. Using ultrasound guidance, the fluid-filled follicles are aspirated with a needle inserted through the vaginal wall. An embryologist then examines the collected fluids under a microscope to isolate the eggs. The eggs are placed into tissue culture dishes with fertilizing medium and placed into an incubator for several hours prior to attempting fertilization. Fertilization is achieved by introducing prepared sperm into the culture dishes, returning them to the incubator, and allowing nature to take its course. In some cases, eggs are fertilized manually by injecting an individual sperm directly into each egg (Inter Cytoplasmic Sperm Injection or ICSI). The resulting embryos will continue to develop for 3 to 5 days, when they will be transferred to the waiting uterus via a catheter inserted through the cervix. In most cases, the intended mother is given hormones to support an optimal uterine lining for implantation.
Fertilizing all the mature eggs retrieved allows for the selection of the best quality embryos for transfer to the intended mother’s uterus. In order to reduce the possibility of triplets or higher-order multiples, the number of embryos transferred is usually limited based on the age of the egg provider and the medical history of the participants. The remaining embryos may be cryopreserved, providing additional opportunities for pregnancy without the expense of an entire IVF cycle. When their family building is complete, some IVF patients generously choose to donate their remaining cryopreserved embryos to someone else who needs assistance in order to conceive.
|
 |
At what stage are embryos frozen?
Embryos may be frozen at any stage of development between 1 and 6 days.
What is an oocyte? Is it the same as a gamete?
An oocyte is an egg. Gamete is a gender-inspecific word that refers to both eggs and sperm.
What is the difference between an embryo and a pre-embryo?
Embryo and pre-embryo are both terms that are used broadly to refer to all the early stages of development of a fertilized egg. The word embryo is specifically used to refer to the stage of development between implantation in the uterus and the 8th week of gestation, so some IVF clinics use the term pre-embryo when describing pre-implantation embryos. However, both words are commonly used to refer to stages of development prior to transfer to the uterus.
|
 |
What is a 2PN embryo?
Male and female gametes (eggs and sperm) each have a nucleus containing DNA. Within hours after penetration by the sperm, the egg jettisons half of its chromosomes in a process called meiosis. (Sperm complete meiosis much earlier, while still in the testes.) The remaining DNA packet from each gamete is called a pro-nucleus. For a period of time after the sperm penetrates the egg, the two pro-nuclei exist separately within the cytoplasm of the egg. Appropriately, this earliest stage of development is called the “two pro-nucleate” (or 2PN) stage. When embryos are being created in an IVF laboratory, the embryologist typically will be looking for proof of initial fertilization (2 pronuclei in close proximity to each other) about 16-18 hours after insemination.
|
 |
What is a Zygote? What are Blastomeres?
Gradually, the two pro-nuclei gravitate toward each other, their cell walls dissolve, and they complete the process of fertilization by merging to form one nucleus. The fertilized egg is now called a “zygote.” The nucleus begins to duplicate itself by dividing into cells called blastomeres. This process is called mitosis. At first, the blastomeres are rather large, but each division produces smaller and smaller blastomeres. Normally, embryos reach the 2-4 cell stage about 24 hours after fertilization (two days after egg retrieval), and a day later, they will have about 8 cells. Here in the United States, Day 3 is the earliest stage at which embryos are routinely transferred to the uterus. In between fertilization and the point at which there are too many cells to count, they are called cleavage-stage embryos. They are also commonly referred to as 6-cells, 8-cells, etc., according to their stage of development.
|
 |
What is a Morula?
When the embryo reaches about 16-32 cells, it is called a morula (mulberry shaped).
What is a Blastocyst?
As the morula continues to divide, it forms an outer shell of cells (the trophoblast) around a fluid-filled cavity (the blastocele) containing an inner cell mass (the embryoblast). At this point, the organism is called a blastocyst. An embryo usually reaches the blastocyst stage around Day 5, which is when it would normally be entering the uterus during a natural cycle. The trophoblast and embryoblast cells will continue to differentiate from one another as cell division continues within the blastocyst, laying the groundwork for the placenta to grow from the trophoblast, and the fetus to develop from the inner cell mass.
|
 |
How does implantation occur?
Around Day 6, the blastocyst will start to “hatch,” or break out of the walls of the egg (the zona pellucida), which can no longer contain the cell division occurring within them. The trophoblast (outer ring of cells) secretes an enzyme which prepares the uterine wall for implantation. Trophoblast cells invade and destroy cells of the uterine lining, creating blood pools to stimulate new capillary growth. Part of the trophoblast will eventually become the placenta, and within 13 days after ovulation, chorionic villi fingers form to firmly attach the developing placenta in place.
|
 |
What is assisted hatching?
Assisted Hatching is a micromanipulation procedure in which a tiny hole is made in the membrane surrounding the embryo (the zona pelllucinda). This membrane holds the blastomeres together, and during natural conception, it helps prevent premature implantation in the fallopian tubes. Normally it disappears right around the time the blastocyst is preparing for implantation in the uterus. Sometime, due to the age of the oocyte provider, or to freezing or other factors, the membrane is thick and the growing blastocyst is unable to break out. In such situations, Assisted Hatching may be employed. Assisted Hatching utilizes either a lazer, or a weak acid solution that is precisely applied, then suctioned away. The embryo is then rinsed to remove any residue of acid, and returned to the culture dish to be further incubated or await transfer. There is an increased risk for identical twins when assisted hatching or other micromanipulation techniques are employed.
|
 |
Is it better to transfer 8-celled embryos or blastocysts?
There is some difference of opinion about whether it is better to transfer embryos on Day 3 (cleavage stage), or Day 5 (blastocysts) The answer may be that it depends upon the protocols of your clinic. Some clinics have not observed a significant difference in pregnancy rates between the two procedures, or speculate that embryos which do not survive to the blastocyst stage in the laboratory might have survived inside the body. However, the argument for incubating embryos longer in the laboratory is twofold. One, it delivers embryos to the uterus at the time they would normally arrive, avoiding exposure to potentially harmful amino acids and carbohydrates. Improvements in culture mediums may provide a more hospitable environment in vitro. Two, it allows for the identification of the strongest, most resilient embryos in the batch, avoiding the possibility that the most viable embryo(s) might be lost during the freezing/thawing process rather than selected for the fresh transfer. Transferring fewer, more robust embryos results in a lower risk of high-order multiple pregnancies (triplets, quadruplets, etc). In many clinics, the transfer of blastocysts results in higher pregnancy rates per transfer, but it also increases the number of couples who do not have any viable embryos at the time of transfer. On average, about 30% of embryos make it to the blastocyst stage, while about 70% stop growing. It is unknown whether these embryos would have survived if transferred earlier, and therein lies the debate. (Actual rates vary between clinics and individual patients. In general, fewer embryos made from the eggs of older patients, and more embryos made from the eggs of donors and younger patients, go on to develop into blastocysts.) Often, clinics will choose extended incubation only when there are sufficient quantities of good quality embryos on Day 3 (8-10 or more) to assure the probability of an adequate number of Day 5 blastocysts for transfer.
|
 |
How are embryos frozen and stored after an IVF cycle?
Very carefully! During the freezing process, even under the stringent protocols used by IVF labs, embryos must survive the dangers of ice formation, extreme changes in temperature, pH and the concentration of electrolyte in their environment, as well as transmembrane water movement.
The cells of embryos, like other living tissue, contain water. Water forms sharp ice crystals and expands as it freezes, which would cause the embryo to burst if it were not removed first. Freezing also builds up high concentrations of salts in water, which would be detrimental to the embryos. In order to prevent this problem, the water is removed from embryos and replaced with cryoprotectant fluid, which does not form ice crystals. The embryos are briefly transferred to a phosphate-buffered medium for 5-10 minutes, then mixed with a highly osmotic cryoprotectant fluid. The embryo temporarily shrinks as it rapidly releases the water in its cells through diffusion. Then it swells back up again as cryoprotectant replaces the water. It only takes a few minutes, and the embryos are ready for freezing. The exact protocols vary from clinic to clinic, but follow a similar process.
Embryos are placed in glass or plastic straws for storage. Typically 1-4 embryos from the same batch are stored in each straw, based on clinic protocols and how many are expected to be thawed and transferred together in the future. The straws are pre-cooled, then placed into canisters that are lowered into temperature-controlled insulated storage tanks (dewars) of liquid nitrogen. The gradual freezing process takes several hours.
|
 |
How long does it take for embryos to thaw?
Embryos thaw to room temperature within less than a minute or two after being removed from cryostorage, but the entire thaw process takes about 40 minutes before the embryo is ready for transfer or further incubation.
How does the thawing process work?
The embryos are removed from their canister and brought to room temperature. In a reversal of the preparation process for freezing, the cryoprotectant is gradually removed and replaced with water by incubating the embryos in increasingly dilute solutions, each containing more water and less cryoprotectant. Again, the embryo may burst when water rushes into the cells, so this process is carefully controlled. Then the embryo is brought to body temperature and transferred or is placed into culture medium in an incubator until transfer. Embryos are normally reevaluated before transfer.
|
 |
Will all the embryos survive the thaw?
How well embryos survive the thaw depends upon the freezing and thawing protocols used and the quality of the embryos before freezing. Embryos graded higher before freezing tend to be more resilient to freezing and thawing. Many clinics will not freeze embryos unless they are of suitable quality. On Day 3, they should have at least 6 cells, and no more than moderate (20-25%) fragmentation, or they are unlikely to survive the procedure. Typical embryo thaw rates vary from 50-80%, with many labs achieving >70% routinely. It is important to ask about the thaw rates at the clinic you will be using.
After thawing, embryos are evaluated. Some will have no surviving cells. These embryos are called “atretic.” Others will be partial survivors, with some cell damage. Large numbers of embryos fall into this category. The damage may be minor or extensive. Though subsequent pregnancy rates do have an inversely proportionate relationship with the extent of damage suffered, these embryos are still capable of resulting in a live birth, and often recover. This was dramatically demonstrated with the very first live birth after a frozen embryo transfer, which occurred in Australia in 1984. The embryo was frozen with 8 cells, but 2 cells were destroyed during freezing/thawing. It was transferred with 6 cells, survived, implanted, and eventually proved to the world that successful human embryo cryopreservation was possible. Since then countless children have been born thanks to this procedure, often after the transfer of embryos that have experienced some degree of cell damage.
The very best quality embryos are those that survive with 100% of their cells intact. It has been suggested that these embryos are essentially as viable as if they had never been frozen, but fewer embryos tend to fall into this category.
Embryos with an even number of cells seem to have an edge over embryos with an odd number of cells; they survive freezing at apx. 5-10% higher rates. Embryos created with donor eggs seem to freeze better than embryos of the same grade created with infertility patient’s eggs; apx. 2-5% more of them survive freezing.
Survival rates may also be affected by the stage of development at which the embryo was frozen. There is some evidence that embryos frozen at earlier stages of development survive freezing better, perhaps because they are simpler in structure and still have an intact nuclear membrane. (For this reason, if there are a very large number of good quality embryos, a portion may be frozen at the 2PN stage, and a portion incubated to produce 8-cells or blastocysts for transfer.) However, it is also postulated that blastocysts may survive better because they have more cells, and therefore can recoup easier from the loss of some of them. In practice, this is a variable that may be lab-dependent, since there are a number of variations to the protocols used for freezing and thawing. What is most relevant is what your clinic has found works for them.
|
 |
How long after they are thawed are embryos transferred?
Blastocysts and embryos frozen at the cleaved stage can be transferred shortly after thawing (0-6 hours), but embryos frozen earlier on are frequently incubated for a day and transferred when they reach the cleaved or blastocyst stage.
How long can embryos be frozen and still be viable?
Theoretically, embryos may be frozen indefinitely, as no biological activity takes place during cryopreservation. In practice, it is unknown how long they can remain viable. The first frozen embryo transfers resulting in live birth took place in the mid-eighties. Since then, embryos frozen as long as 12 years have resulted in successful pregnancy. Freezing and thawing protocols continue to improve, making it possible that embryos frozen more recently may have better outcomes.
|
 |
Will frozen embryos be as likely to produce a pregnancy as fresh embryos after they are thawed?
The success rates for frozen embryo transfers are usually lower than those for fresh embryo transfers. This may be due to damage to the embryos during freezing, but may also be due to the fact that the embryos evaluated to be of the highest quality in the batch are usually transferred fresh. In addition, more patients undergoing a frozen embryo transfer have had a failed cycle than those undergoing a fresh transfer.
|
 |
Can embryos be frozen more than once?
Yes. Sometimes when a large quantity of embryos are frozen at an early stage of development (2PN), all or a good number of them will be thawed and incubated. As with a fresh transfer, the best quality embryos will be selected for transfer and the remainders re-frozen. Live births have resulted from the transfer of twice-frozen embryos, but some of the same factors that make frozen embryos transfers less effective than fresh transfers would be expected to reduce the success rates for refrozen embryos.
|
 |
What are the factors thought to affect embryo quality?
Age of egg provider
Method of ovarian stimulation
Timing of ovulation trigger
Length of ovarian resting time since last IVF cycle
Quality of Sperm (DNA fragmentation, etc)
Embryology Laboratory protocols and expertise (including culturing environment)
Smoking
Weight
Polycyctic Ovarian Syndrome
What is fragmentation?
Embryo fragmentation occurs when cells divide unevenly, creating bits of membrane-bound cytoplasm that have no nucleus. The majority of embryos created during IVF cycles are observed to have some fragmentation, however, the more fragmentation, the less likely an embryo is to develop normally and implant successfully. The extent of fragmentation is an important indicator of embryo quality. Some research has also shown that the size of fragments also has an effect on embryo viability.
|
 |
How are embryos graded?
Different clinics use different grading systems, so it is important to ask what system is used at the clinic where the embryos were created. Either a numerical or alphabetical grade is given based on the rate of cleavage and overall quality. A 3, 4 or 5-point scale may be used. Quality is most often evaluated based on appearance, but a few labs are now using a more sophisticated chemical marker test (sHLA-G) to identify the embryos with the best potential for implantation. Generally speaking, a better quality embryo is more likely to survive freezing than a poor quality embryo created on the same day.
In a typical scheme in which embryos are graded from 1 to 4 (with Grade 1 being the best), Grade 1 embryos are morphologically perfect, with round, symmetrical cells. They have the appropriate number of cells for their stage of development. Cell division is even, and there is no visible fragmentation. Only 20% of embryos receive the highest grade. Most embryos have slight imperfections, and this is normal and expected. Grade 2 embryos have the correct number of cells for their developmental stage, and usually have even cell division. They might have slight unevenness of blastomere sizes and/or a small amount of fragmentation (<20%). Grade 3 embryos have uneven cell division and moderate fragmentation (>30%), or are behind in their development, or have similar irregularities. Grade 4 embryos have uneven cell division and extensive fragmentation (>50%). They may have few viable cells or be completely fragmented. Generally, embryos graded at the bottom of the scale are associated with poor chances for a viable pregnancy. Keep in mind that this is just an example of a grading system. The actual parameters used to evaluate embryos vary somewhat and grading is subjective.
At some clinics, blastocysts are graded with a number and two letters. The number refers to the amount of expansion, the first letter to the quality of the inner cell mass that will develop into a baby, and the second letter to the quality of the outer cell mass that will become the placenta. Again, it is best to check with the clinic where the embryos are created for an explanation of the grading system used.
|
 |
What is “normal development” for an embryo at the time of transfer?
Hours after insemination or ICSI:
4 cells by 48 hours
8 cells by 72 hours (3 days)
Morula stage by 96 hours
Blastocyst formation by 120 hours (5 days)
|
 |
What is PGD?
Preimplantation Genetic Diagnosis (PGD) involves microsurgical removal of one or two blastomeres from a 6 or 8 cell embryo (generally on day 3). Removal of a cell at this point in time does not appear to harm the embryo. Various technologies are then employed to test the embryo for chromosomal abnormalities. When appropriate, cells from the egg’s polar body may be tested instead and these cells can be removed much earlier. The polar body, which normally dissolves at implantation, does not have any known role after fertilization, so this is considered less invasive.
PGD can be used to detect chromosomal abnormalities or problems with genetic coding that will lead to later miscarriage or heritable diseases. Allowing embryos to develop to the blastocyst stage before transfer weeds out most monosomies (embryos with one, rather than two, copies of a chromosome). These embryos tend to cease developing early on, around day 4. Trisomies (embryos with three copies of a chromosome, as in Down’s syndrome) account for about one forth of all spontaneous abortions. They may look just like other embryos, so PGD is used to identify them.
PGD-FISH (fluorescent in situ hybridization) can detect extra, missing or translocated chromosomes. PGD-PCR (polymerase chain reaction) can identify specific mutations such as those causing Cystic Fibrosis, Tay-Sachs disease, sickle cell anemia, muscular dystrophy, and X-chromosome linked disorders. When PGD-PCR is used, the genetic code in the selected blastomere is duplicated many times over so that it is possible to detect the genetic code that would result in a particular disorder.
Testing usually takes 24-48 hours, after which embryos can be selected for transfer based on the information gained. PGD is not foolproof, because some embryos contain both normal and abnormal cells (a condition called mosaicism) and the particular cell selected for testing may not be representative. But it is a very useful tool, with accuracy between 90-98%. Where there are no chromosomally normal embryos, the chances of a live birth are low. This happens most often when the egg provider is over 40. PGD can increase the cost of a cycle by $2,500 and $5,000.
|
 |
Is it possible to have genetic tests performed on embryos that have been frozen?
Yes, PGD may be performed after the embryos are thawed.
Is it possible to tell the gender of an embryo?
Yes. PGD (see above) can also be used to determine sex based on chromosomes (XX for females; XY for males). Gender selection may be used to avoid certain genetically transmitted diseases that are only carried by male or female offspring. The Ethics Committee of the American Society of Reproductive Medicine (ASRM) discourages the use of PGD to select gender for non-medical reasons. Couples who are seeking to balance their families with a child of a specific gender may also use techniques like sperm sorting (i.e., MicroSort) to increase their odds of the hoped-for outcome.
|
 |
What is the typical success rate with frozen embryo transfer?
The Centers for Disease Control and Prevention (CDC) publishes an annual report on Assisted Reproductive Technology (ART) statistics in the United States. The information is self-reported by participating fertility clinics. The most recently published report, from 2002, indicates that the live birth rate for transfer of frozen embryos created with non-donor eggs is 28%, and when the embryos were created with donor eggs it is 38%. The report does not contain information on the success rates for donated frozen embryos, but it would be reasonable to expect that similar success rates would apply, depending on whether the embryos were originally created with donor eggs or an IVF patient’s eggs.
|
 |
When do embryos implant in the uterus?
During a natural cycle resulting in conception, an egg released from the ovary is fertilized by sperm in the fallopian tube, and arrives at the uterus 3 to 5 days later. If it is still at the morula state when it enters the uterus, it will take a day or two to develop into a blastocyst. Either way, implantation normally occurs 5-8 days after fertilization, with day 6 being the most common day. During IVF cycles, effort is taken to simulate the natural state of affairs, so that the uterine lining is in synch with the development of the embryo and receptive to implantation. Frozen embryos are usually transferred on Day 17 or 19 of a menstrual cycle (depending on the developmental stage of the embryos).
What are the symptoms of implantation?
Some women experience light bleeding (spotting) or cramping at the time of implantation, but others feel perfectly normal. The only way to initially tell if implantation has been successful is to take a pregnancy test.
|
 |
How soon can I take a pregnancy test?
Pregnancy tests measure human chorionic gonadotropin (hCG) which is produced by the placenta during pregnancy. Home pregnancy kits test for hCG in urine; professional beta serum pregnancy testing measures hCG in the blood. The sensitivity of home pregnancy tests varies from as low as 15 mIU/mL to 100 mIU/mL or higher, whereas some beta tests can detect hCG in the blood as low as 5 mIU/mL, which can occur within a week of embryo transfer. (<5% is considered negative; >25% is considered positive) 85% of the time, in the early stages of a normal pregnancy, hCG levels double about every 48-72 hours. Since many doctors require their patients to wait two weeks after their transfer before administering a beta blood test, a sensitive home pregnancy test can often be used for first confirmation of pregnancy.
|
 |
What factors can be used to assess the likelihood that an FET will be successful?
The three most important factors affecting FET pregnancy rates have been shown to be:
Embryo grade after thaw
Number of embryos transferred
Number of embryos transferred with 100% cell survival after thaw
Factors that may come into play include:
Age of the ovum provider at the time of egg retrieval
Sperm quality (factors like DNA fragmentation begin to affect development after Day 3)
Embryo grade and cell division prior to freezing (affects survival)
Stage of development at time of transfer (slightly higher rates of implantation for blastocysts)
Whether assisted hatching was performed (some evidence this improves implantation rates for previously frozen embryos)
Uterine environment (bloodflow, miomas, uterine birth defects, malfunction of the cervix, endometriosis, immune issues, infections and various other factor may affect implantation)
Whether a live birth resulted from the fresh transfer for the same batch of embryos.
|
 |
Are children born from frozen embryo transfer normal?
The cryopreservation process does not appear to adversely affect birthweight, perinatal mortality rates, birth defects, growth or health of children during infancy and early childhood over children born from fresh IVF transfers. However, the long term affects of cryopreservation over a lifetime have not been studied extensively in humans, and since this technology is only about twenty years old, most of the children whose parents utilized cryopreservation are still in the process of growing up.
|
 |
|
| Bibliography: |
A Case of Identical Twins, Richard Bronson, MD (PrevMed, Volume 6, No. 3, March 1998)
Assisted Hatching PregnancyMD.org website (2001)
A quantitative analysis of the impact of cryopreservation on the implantation potential of human early cleavage stage embryos, D.H. Edgar, H. Bourne, A.L. Speirs, and J.C. McBain (Human Reproduction, Vol. 15, No. 1, 175-179, January 2000)
Assisted Reproductive Technologies (ART) GYFT Clinic Website.
At What Stage Can Embryos Be Frozen? Family Beginnings (2005)
Birth characteristics and perinatal outcome of babies conceived from cryopreserved embryos, I Wada, MC Macnamee, K Wick, JM Bradfield and PR Brinsden (Human Reporduction Vol 9, 543-546)
Births of normal daughters after MicroSort sperm separation and intrauterine insemination, in-vitro fertilization, or intracytoplasmic sperm injection. EF Fugger, SH Black, K Keyvanfar and JD Schulman (Human Reproduction, Vol 13, 2367-2370, 1998)
Blastocyst Stage Embryo Transfer, Genetics and IVF Institute (1995-2004)
Blastocysts Vs. Day 2-3 ET - How Strong Is the Evidence? D.K. Gardner and W.B. Schoolcraft (2001, The Second Congress on Controversies in Obstetrics, Gynecology and Infertility, Paris. Monduzzi Editoire, Bologna. pp 259-265.)
Choosing the Best Embryos for Transfer, Geoffrey Sher, M.D.
Clinical factors for successful cryopreserved-thawed embryo transfer. Kondo I, Suganuma N, Ando T, Asada Y, Furuhashi M, Tomoda Y. J Assist Reprod Genet. 1996 Mar;13(3):201-6.
Cryopreservation of Early Cell Stage Human Embryos. G. Goldsmith, A. F. Baker, K. Nowroozi, and J. H. Check
Does assisted hatching pose a risk for monozygotic twinning in pregnancies conceived through in vitro fertilization? Schieve LA, Meikle SF, Peterson HB, Jeng G, Burnett NM, Wilcox LS. (Fertility and Sterility 2000 Aug;74(2):288-94).
Early Pregnancy Including HCG Leveles and Ultrasound Findings, Advanced Fertility Center of Chicago (2005)
Embryo “Competence” and the Embryo Marker Expression Test (EMET), SIRM (2005)
Embryo Cryopreservation Storage, Reproductive Science Institute (2003)
Embryo Cryopreservation, Michael S. Opsahl, M.D. (Genetics & IVF Institute Newsletter, Vol 16, No 3, Summer 2002)
Embryo Donation- A Family Building Option – A Guide for Professionals (RESOLVE)
Embryo Freeze and Transfer, Victoria Fertility Centre (2004)
Embryo freezing: is it safe? Maureen Wood, research embryologist, Department of Obstetrics and Gynaecology, Aberdeen. (BioNews,2004)
Embryo quality and pregnancy potential of fresh compared with frozen embryos--is freezing detrimental to high quality embryos? Selick CE, Hofmann GE, Albano C, Horowitz GM, Copperman AB, Garrisi GJ, Navot D. (Human Reproduction 1995 Feb; 10(2):392-5)
Freezing of human sperm, oocytes and embryos, Pacific Fertility Center (2005)
Gamete and Embryo Quality, Role in fertilization failures and reproductive pathology: the contribution of Fluorescent In Situ Hybridization (FISH) M. Benkhalifa and Y. Menezo (Geneva Foundation for Medical Research and Education, 2003)
Glossary of Terms Used in Assisted Reproductive Technology (Fertility Associates, Medic8 Family Health Guide, 2005)
HLA-G, an Ace up the Sleeve? M. Urosevic, R. Dummer, (ASHI Quarterly, Third Quarter, 2002)
Home Pregnancy Test hCG Levels and FAQ, Fertility Plus website (2003)
Human Chorionic Gonadotropin (hCG), the Pregnancy Hormone, American Pregnancy Association (2004)
Human Embryo Cryopreservation (Embryo Freezing) and Frozen Embryo Transfer Cycles, Genetics and IVF Institute (2004)
Human embryo fragmentation in vitro and its implications for pregnancy and implantation. Alikani M, Cohen J, Tomkin G, Garrisi GJ, Mack C, Scott RT. (Fertility and Sterility, 1999 May;71(5):836-42.)
Human Oocyte and Embryo Cryopreservation, Michael J. Tucker, PhD, Georgia Reproductive Specialists (2003)
Influence of oocytes and spermatozoa on early embryonic development. Salumets A, Suikkari AM, Mols T, Soderstrom-Anttila V, Tuuri T. (Fertility and Sterility 2002 Nov;78(5):1082-7.)
IVF Embryo Culture and Blastocyst Transfer, IVF1.com website
Live-birth rates and multiple-birth risk of assisted reproductive technology pregnancies conceived using thawed embryos, USA 1999–2000 Anjel Vahratian1, Laura A. Schieve, Meredith A. Reynolds and Gary Jeng (Human Reproduction, Vol. 18, No. 7, 1442-1448, July 2003)
Medical Cell Biology: Fertilization and Implantation. Jeanne M Snyder, PhD; Lecture, Department of Anatomy and Cell Biology, University of Iowa (2001)
Merck Manual of Medical Information, second home edition
Monozygotic wtinning following assisted conception: an analysis of 81 consecutive cases. M. Alikani, N.A. Cekleniak, E. Walters and J. Cohen (Human Reproduction, Vol. 18, No. 9, 1937-1943, September 2003)
Morphological Scoring of Human Embryos and Its Relevance to Blastocyst Transfer. (Michael J Tucker, Georgia Reproductive Specialists, 2003)
PGD Questions and Answers (Center for Advanced Reproductive Services website)
Poor Egg/Embryo Quality: An Important Cause of In Vitro Fertilization Failure. (Sher Institute of Reproductive Medicine, 2005)
Postnatal growth and health in children born after cryopreservation as embryos.Wennerholm UB, Albertsson-Wikland K, Bergh C, Hamberger L, Niklasson A, Nilsson L, Thiringer K, Wennergren M, Wikland M, Borres MP. (Lancet. 1998 Apr 11;351(9109):1085-90.)
Preimplantation Genetic Diagnosis (PGD), Arizona Center for Reproductive Endocrinology and Infertility website.
Preimplantation Genetic Diagnosis (PGD). Barry Behr, PhD, HCLD & Victor Ivakhnenko, HCLD (Huntington Reproductive Center website)
Pre-Implantation Genetic Diagnosis: How it changes the IVF experience. Beth Ary, M.D., FACOG, Reproductive Endocrinologist Reproductive Specialty Medical Center
Prognostic factors for the success rate of embryo freezing. PO Karlstrom, T Bergh, AS Forsberg, U Sandkvist and M Wikland, Human Reproduction, Vol 12, 1263-1266 (1997)
Prognostic factors of implantation, D. de Neubourg (J Gynecol Obstet Biol Reprod/Paris, 2004 Feb;33[1 Pt 2]:S21-4.)
Sex Selection and Preimplantation Genetic Diagnosis; The Ethics Committee of the American Society for Reproductive Medicine (Fertility and Sterility Vol 72 No 4, Oct 1999)
Science Pulse: How Emrbyos Make the Grade. (Fertility Flash Vol 3 Issue 5, May 2005)
The Visible Embryo (viseembryo.com)
Thinking About PGD Chelsey Langland (StorkNet)
Twin delivery following 12 years of human embryo cryopreservation: Case report. A. Revel, A. Safran, N. Laufer, B.E. Reubinov and A. Simon (In Vitro Fertilization Unit, Department of Obstetrics and Gynecology, Hadassah University Hospital, Ein Kerem, Israel)
University of New South Wales (UNSW) Embryology website, Dr. Mark Hill (2005)
Why Should We Assess Oocyte and Embryo Quality? (KE Tucker, CAM Jansen, Proceedings 2nd International workshop for Embryologists: Troubleshooting Activities in the ART Lab, 2002)
|
 |
|
|
| The Miracles Waiting, LLC. Team |
The Information provided in this page is for educational purposes only and you should not rely on it as a substitute for professional assistance. If you are concerned about your health or the health of a loved one please seek the help of a medical care provider.
|
|
|
|
 |
|
|
 |
|
|
|
Nearly 400,000 embryos are stored in the United States,
88.2% are targeted for patient use, and
2.8% are available for research.
FERTILITY AND STERILITY |
|
|
